Healthy senior nutrition begins with knowing how your food intake affects your health outtake.
Recognize the signs of weight loss and declining appetite
Weight loss is generally considered a symptom of healthy eating; this makes it more difficult to recognize anorexia in the elderly as a serious health risk. Also concerning: many studies show a link between preferences for unhealthy foods and diminished mental abilities. Individuals may seem confused and forgetful, listless, and easily fatigued—these can be signs of malnourishment, rather than cognitive decline.
Nutrition is cell science
Nutritional needs change over the years. Metabolisms slow, and aging bodies require more of certain key nutrients. Poor nutrition increases the risk of chronic diseases associated with aging, such as heart disease, stroke, type-2 diabetes, bone loss, and cancer. Proper nutrition contributes to the healthy functioning of cells at the most basic level and can boost mental acuity, retard the effects of debilitating bone loss and arthritis, and help to manage cholesterol and blood pressure. Healthy eating gives cells the fuel they need to keep going.
The elderly sometimes lose their appetite. Dulled taste buds, uncomfortable dentures, and medications may have an effect but loneliness can be the most insidious. In some cases, just the prospect of eating is unpleasant.
Physical signs of poor senior nutrition
Sometimes, a senior appears well-fed yet is starved of nutrients. Aches, pains, and lethargy may be mistaken as the natural effects of aging when, in fact, they are symptoms of nutrient deficiencies. In considering a person’s overall need for assistance, caregivers can look for physical signs that an older individual’s diet is not sufficiently nutrient-rich. Here are only a few physical signs of poor nutrition:
- Muscle weakness, constipation, tingling, and numbness may point to a potassium deficiency. Bananas, whole grains, milk, beans, and peas are important sources of potassium.
- Fatigue, pale skin, and thinning, dull hair may indicate low iron levels needed to produce red blood cells.
- Brittle bones, fatigue, and muscle aches might indicate low Vitamin D levels. Introduce more fatty fish, yogurt and other fortified dairy products into the diet, and spend more time in the sun.
- Vegans might experience a Vitamin B 12 deficiency: hard to detect until it becomes severe when it manifests as wobbliness, weakness, memory loss, and even hallucinations.
- Dry skin, macular degeneration, ridges in nails are associated with a Vitamin A deficiency. Carrots (and other orange vegetables) and dark green leafy vegetables boost Vitamin A.
Check with a physician prior to starting a new diet or making significant dietary changes. It is also important to be aware of any foods that should be avoided due to medications.
Household clues of poor senior nutrition
Often a household will provide other clues of poor senior nutrition, such as:
- Opened, but expired food products in the refrigerator and unopened but expired products in cupboards
- No indication of recent cooking activity such as a clean kitchen and empty dishwasher or, conversely, dishes and pans that haven’t been washed in days
- A cupboard full of energy-dense but nutrient-poor foods, such as crackers, chips, cookies, etc. and, in the absence of fresh fruit and vegetables, canned and highly processed pre-prepared meals
- The volume and kind of trash generated over the course of a week
When an older individual resides independently at home, there are ways to ensure that the right amount and kind of foods are available. In-home delivery services, such as Peapod, make it possible to order online. Many of these services also carry ready-prepared food “kits”, although sodium content on these kits should be examined. When possible, caregivers can stock freezers with more healthy alternatives or call on a community’s aging services such as Meals on Wheels.

Healthy Eating Tips for Seniors
Understand that budget plays a role
Where budgets are stretched, fast food or “blue plate specials” can be less costly than a trip to the grocery store. This link between low income and unhealthy eating is well-documented. Especially when disabilities limit mobility and capability, regular and well-balanced meals are not possible. The cumulative effect can be devastating: the poorer an individual’s diet, the more important nutrition becomes to good health.
Choose fresh foods instead of packaged meals
It takes a lot of chemicals to preserve a package of prepared food and they do not magically disappear when consumed. Food additives are processed by the liver which is already working overtime on 500 vital functions, including sorting through our blood flow for other toxins. Be cautious by taking the words “shelf life” literally and leaving pre-packaged foods laced with preservatives on the store shelf.
Columnist Gary Larson put it well: “life expectancy would grow by leaps and bounds if green vegetables tasted like bacon.” The fact is that, whatever we are eating, we are probably not eating enough vegetables. Veggie-rich diets lower blood pressure, reduce calorie intake, and lower the risk for every ill from macular degeneration to heart disease. In fact, leafy greens top the list for Vitamin K (a defense against osteoporosis), Lutein (eye health), and magnesium (diabetes fighter). And seniors especially should not skimp on their vegetables. Nourish hungry cells by filling half of every plateful of food with vegetables and munch away with a clear conscience.
Look out for sugar, salt, and saturated fats
Combinations of flour, sugar, salt, and saturated fats are just so delicious and just so unhealthy; they are food’s sly villains! All sorts of chronic diseases result from the preponderance of these ingredients in a daily diet. Healthy senior nutrition means limiting saturated fats to not more than 10% of daily calories and avoiding trans fats as much as possible. People who cut these out of their diets report that after a while, they find processed foods containing trans fats greasy and unappealing.
Honor tastiness
The cells within those 10,000 or so taste buds you had at birth also wear out (oh dear). Plus, certain medications and medical issues may affect how well taste sensations—closely allied to the sense of smell—are carried to the brain. As we age, spices and other seasonings—not salt—marinades, dressings, and flavored sauces can make food more appetizing. Meal presentation also plays a part: colorful ingredient combinations, attractive plating, and special garnishes add piquancy and interest.
Recognize eating habits
Eating habits are well-established long before the first social security check, but they can evolve as we age, and not always for the better. Liberated from the day-to-day demands of family life, many seniors change their cooking habits or stop cooking entirely. For some, dining out becomes a daily routine, providing opportunities to socialize, but, in the process, adding calories to the diet and inches to the waistline.

Menu Planning for Seniors
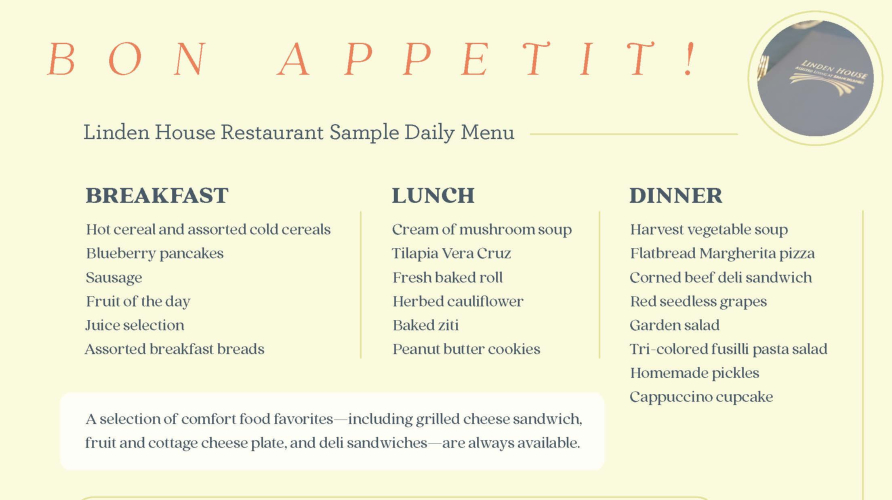
Menu quality is a critical factor in sustaining the health of residents in a senior living community. Nutritionists must address potential interactions with medications and food allergens. Menu variety ensures that seniors look forward to meal time. Fresh ingredients deliver nutritional content. Textures and flavors must appeal to muted taste sensations.
It’s a tall order, but nutritionists who specialize in senior nutrition have the expertise to put it all together.
Fresh and delicious dining at Branchlands
The quality of meal services is one of the most important considerations when selecting a senior living community. The idea is surprise and delight, not bland and boring! The best senior communities have staff nutritionists and chefs collaborating to ensure quality, freshness, and variety. Meal planners also consider religious preferences, special dietary needs, allergies, and dysphagia (trouble swallowing).
Our delicious menu uses local, in-season food to keep our menu fresh and nutritious. Our chefs work with residents to provide a varied menu of scratch-made meals that has something for everyone. We even use our own resident recipes for featured meals. For our residents with cognitive needs, our Memory Care menu is designed to enhance abilities and help our residents maintain independence with dining.
To learn more about how Branchlands ensures quality dining, contact us to make a dinner reservation.